How to ensure your staff are administering medication safely-r’s of medication

Included:
7 R’s of Medication Administration
Care staff are often called upon to deliver medication in health and social care settings. In this case, paying attention to the 7 rights of medication becomes very important. This is also referred as the 7 r’s of medication administration.
Staff often face the challenge of administering medication accurately amidst busy schedules and competing demands from patients.
There are a number of key areas staff need to ensure they understand when administering medication, and it’s useful for them to have reminders of this alongside any training given, to keep refreshing best practice.
Table of contents
- Controlled and uncontrolled drugs
- Different routes of medication
- The seven Rs: What are the 7 r’s of medication administration?
- Why is the 7 rights of medication administration important?
- Checking the MAR Chart and Medical Labels
- How the Medication R’s Expanded to 10 R’s of Medication.
- So what are the 10 rights of medications?
- Documenting medication administration correctly
- Medication errors
- What Next? Accessing the right training for safe medication
- LATEST POSTS
Key Learnings: The seven rights of administering medicines are: Right patient, right medication, right dose, right route, right time, right documentation, right reason. They are very important for care workers, nurses, support workers and other health officials responsible for different types of administering medicines.
Controlled and uncontrolled drugs
Misuse of drugs legislation explains in full extent how to use and handle controlled drugs. Meaning you can treat them differently from uncontrolled drugs. Examples of controlled drugs are morphine patches, and benzodiazepines e.g. diazepam.
Staff must be aware of the specific storage and administration requirements for controlled drugs, ensuring that they know how to handle and administer these medications properly.
Your organisation should have a medication policy, and there should be a specific section on controlled drugs:
- who will administer them,
- how they are administered,
- where they will be stored,
- how they will be disposed of and who has access to them.
Our Safer Management of Medicines course will talk you through everything you need to know about controlled drugs.
Different routes of medication
There are a number of ways medication can be given. Most patients take their medication orally, in tablet or liquid form.
These are not the only ways. There are ways.
Common routes of medication in health and social care include:
- Transdermal – Through a patch, for example a pain relief or a smoking cessation patch.
- Topical – Often used in social care – such as a cream applied to the skin
- Rectal – Medication inserted into the rectum through a suppository or enema.
- Otic – Administered by drops into the ear
- Ophthalmic – Placed in the eye through drops, a gel or an ointment
Social care settings, such as residential care and nursing homes, often use controlled drugs. Common examples include the following. There are a number of other routes of medication which we’ll cover on the course.
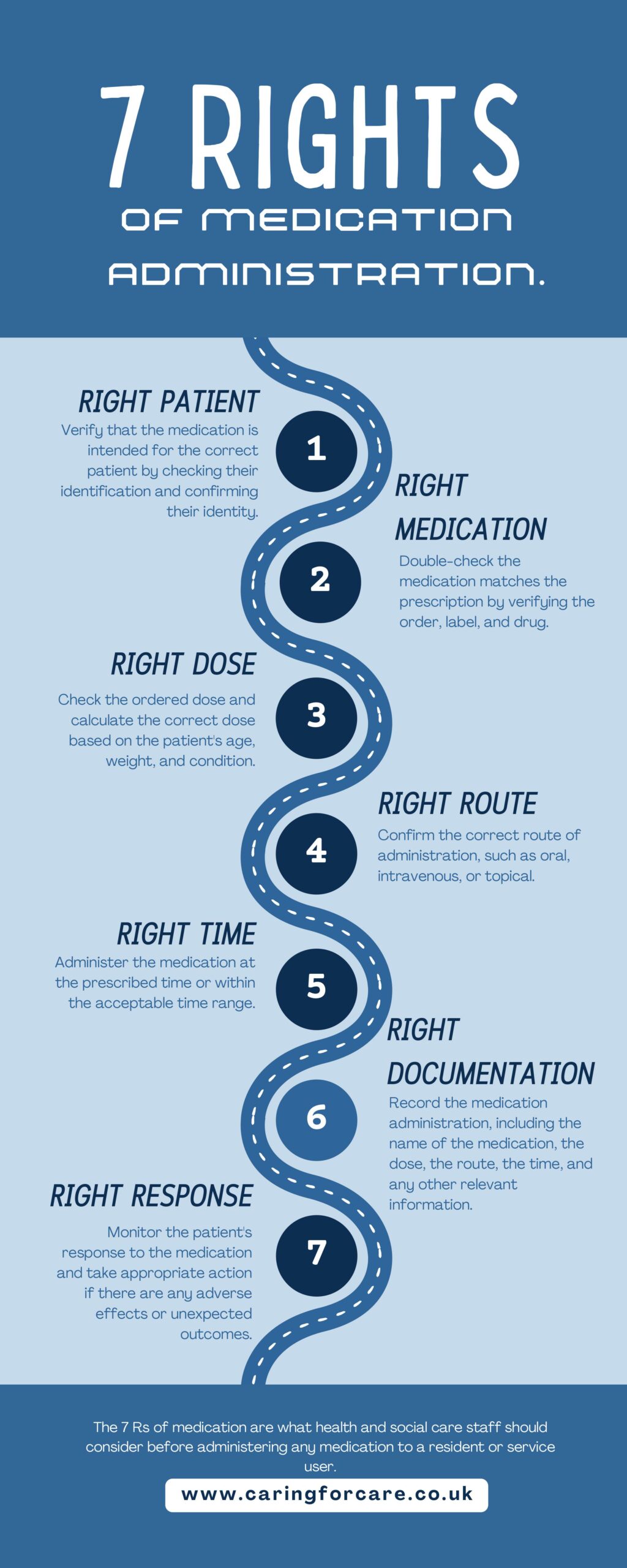
The seven Rs: What are the 7 r’s of medication administration?
This is a really good reminder for staff to get medication administration right.
The seven rights of administration of medicine are what health and social care staff should run through before administering any medication to a resident or service user.
- Right patient: Verify that the medication is intended for the correct patient by checking their identification and confirming their identity.
- Right medication: Double-check that the medication is the correct one that was prescribed by checking the order, label, and medication. Wrong medication may result in side effects and severe complications. So, be sure to give the correct medications always.
- Right dose: Check the ordered dose and calculate the correct dose based on the patient’s age, weight, and condition. check and recheck to be certain that the correct dose is given.
- Right route: Confirm the correct route of administration, such as oral, intravenous, or topical.
- Right time: Administer the medication at the prescribed time or within the acceptable time range.
- Right documentation: Record the medication administration, including the name of the medication, the dose, the route, the time, and any other relevant information.
- Right response: Monitor the patient’s response to the medication and take appropriate action if there are any adverse effects or unexpected outcomes.
The seven R’s of administering medication serve as a robust framework that emphasizes patient safety, accurate care delivery, and effective communication in healthcare settings.
Interested in Medication Administration? Get in touch with our course advisors at 01782 563333 or email us at enquiries@caringforcare.co.uk for course information and expert guidance on your healthcare journey.
Infographics: 7 R‘s of administering medicines
Why is the 7 rights of medication administration important?
The right of medication administration is of utmost importance as it forms the foundation for safe and effective healthcare practices. Ensuring the right of medication administration involves adhering to essential principles before giving any medication to a patient.
The importance of the right of medication administration lies in several key aspects:
- Patient Safety: Adhering to the five r’s significantly reduces the risk of medication errors, prioritizing patient safety above all else.
- Effective Treatment: Administering the right medication (also right type of medication) in the correct dose and route at the proper time enhances treatment efficacy, leading to improved health outcomes.
- Avoiding Adverse Reactions: The right of medication administration helps prevent adverse drug reactions that could arise from using the wrong drug or incorrect dose.
- Building Trust: Demonstrating a systematic and careful approach to medication administration builds trust with patients, promoting treatment adherence.
- Legal and Ethical Obligations: Following the five Rights aligns with legal and ethical responsibilities, ensuring compliance with professional standards of care.
- Reducing Healthcare Costs: Avoiding medication errors through the right of medication administration can save healthcare systems from the financial burdens associated with managing adverse events.
- Professional Development: Emphasizing the importance of the right of medication administration encourages continuous education and professional growth, fostering competence and accountability.
Checking the MAR Chart and Medical Labels
Essentially a staff member is checking that they have the right drug and dose based on a person’s records. They also need to check that the person in front of them is also the person the medication is for.
A good way of doing this is to have a recent photograph with the medication administration record (MAR) chart. Then, check this against the person in front of them.
The person administering also needs to check the medication label and MAR chart to make sure they are giving the medication at the right time of day.
Administering some medication requires strict timing, such as every four hours, thus it is crucial to check the timings before administering.
The right route is checking that the resident should be receiving the medication orally or topically, and making sure that is what they are administering.
The label from the GP, which staff should have printed or copied onto the MAR chart, should have this information.
The staff member needs to make sure they also have the right MAR charts for the person they are giving medication to.
So checking name and DOB for example against a care file. Staff members should check the chart in front of them before administering, as staff sometimes make up charts in advance.
Finally, the resident has a right to refuse to take their medication.
Sometimes we give medication covertly, but only in exceptional circumstances with prior involvement from a GP and after associated capacity processes and best interest decisions have occurred.
Otherwise, if a person refuses medication, we should document the refusal and seek medical or management advice.
Always Double-Check and Document
Recent development on medication: 8r’s of medication:
The eight R’s of medication is the “right to refuse”.
It refers to the patient’s right to decline or refuse medication or treatment. Even if a healthcare professional has prescribed it.
As healthcare providers, it is important to respect the patient’s choices and freedom.
It is important to provide them with information about the risks and benefits of the medication or treatment. Including any alternative options that may be available.
The healthcare provider should closely monitor patients who refuse medication or treatment and consider alternative interventions if appropriate.
We should discuss the 5 Rs of medication administration or the 7 Rs of medication administration, but the right documentation is just one more addition to the rights of medication administration.
READY TO BECOME A CERTIFIED MEDICATION TRAINER? JOIN OUR NEXT CLASS
How the Medication R’s Expanded to 10 R’s of Medication.
The origins and use of the 10 Rights of Medication Administration are not entirely clear from research. However, here is a summary of the history of these rights.
- The core concept of “rights” in medication administration has existed for decades, though earlier versions had fewer elements.
- By the 1960s, nursing practice had agreed on the five rights (right patient, drug, dose, route, time) and widely used them in nursing education.
- By the 1980s, sources referenced additional rights, like right documentation and reason, bringing the list to 7 Rights.
- During the 1990s, the full 10 Rights expanded to also include right action/method, response, refusal, and education.
- The 10 rules for giving medicine were widely followed in nursing and medication safety practices by the 2000s. Some sources cite the Joint Commission incorporating them into standards by 2006.
- While expanded over the years, the 5 original Rights have remained foundational.
So in summary, while an exact origin is unclear, the core five rights existed for decades before gradually expanding to the comprehensive 10 Rights framework we know today, with key developments occurring in the 1980s and broader adoption during the 1990s and 2000s.
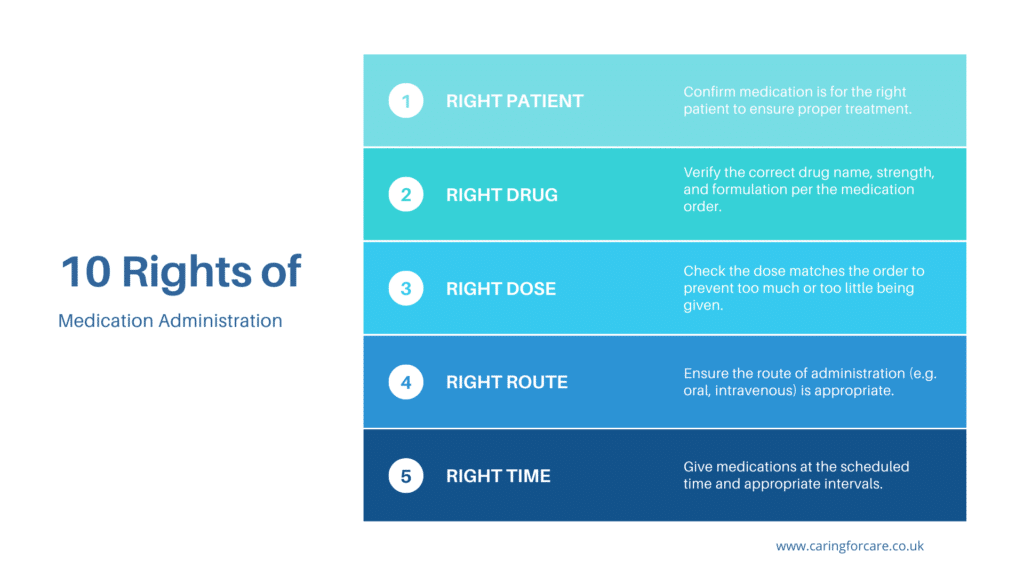
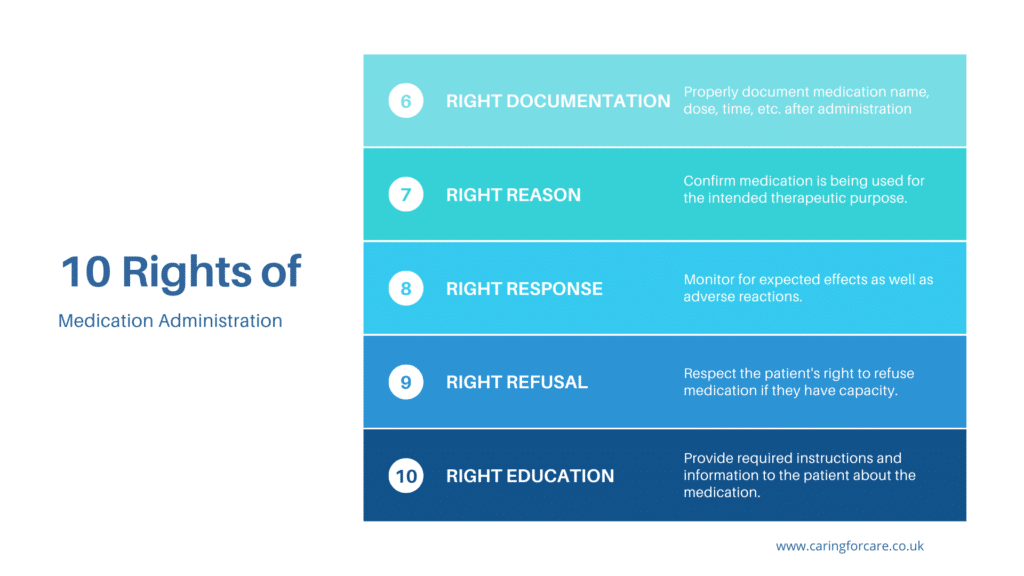
So what are the 10 rights of medications?
Healthcare workers follow the 10 r’s for giving medicine to make sure they give the right medicine to the right person at the right time.
These rules protect patients, respect their rights, and make sure the medicines are right for their needs.
Knowing and following these rights of medication is important for providing good healthcare.
- Right Patient – Confirm patient identity matches the name on the medication label using two labels (e.g. name, DOB, medical record number). Prevents potential adverse events from giving medications to the wrong patients.
- Right Drug – Check medication name, strength, and formulation on label with the medication administration record (MAR) to ensure the exact prescribed drug is administered. Prevents medication errors.
- Right Dose – Verify prescribed dose on MAR matches dose prepared for administration to prevent over or under dosing errors. Right formulation is also key.
- Right Route – Check appropriate route (IV, oral, topical etc) is used for administering medication. Following correct route is vital for calming effect and safety.
- Right Time – Give medications at prescribed times or within defined time windows (e.g. within 30 minutes before or after scheduled time) to maintain therapeutic levels.
- Right Documentation – Charting details like medication name, dose, route, time in patient record provides legal proof of treatment delivery while tracking response.
- Right Action – Perform all preparation, double-check, administration, and monitoring steps correctly according to clinical standards and hospital policy.
- Right Reason – Verify medication indication or diagnosis to ensure proper therapeutic usage vs unapproved usage without clinical indications.
- Right Response – Assess for expected therapeutic effects as well as adverse events or reactions after administration to determine medication is tolerated and working.
- Right Education – Provide required instructions about medication use, precautions, side effects, storage etc. to the patient for safe and appropriate usage.
Documenting medication administration correctly
We’ve talked about the importance of documenting administration correctly. This is for a number of reasons.
The health and care regulator, the Care Quality Commission (CQC) will check the documentation on inspection, and this could affect the rating that your organisation receives.
In controlled drug use, incorrect documentation can also lead to breaking the law.
On a more day-to-day level, a robust documentation system will benefit both staff and residents as shifts change and different people receive training to administer medication.
Lots of pharmacies offer a computerized MAR chart administration system; otherwise, clear recording in black pen, using an agreed coding system, is key.
You will then be able to demonstrate to the relevant authorities such as your local commissioners and to CQC that you understand medication administration and you are getting it right.
LIMITED TIME OFFERS – UPSKILL WITH ONLINE CLINICAL COURSES – CPD CERTIFICATE APPROVED
Medication errors
People do make mistakes, and sometimes a medication error may happen. It’s important that your staff feel able to admit when they’ve made a mistake.
Your policy should cover what happens in the event of an error. The staff should contact either the person’s GP or NHS 111. This is to ensure there will not be an issue if a dose is missed or given incorrectly.
The person responsible should record this advice in the person’s notes.
In instances of incorrectly completed documentation, re-training is often crucial. It ensures that your staff not only gets it right in the future but also comprehends the importance of accurate documentation.
What Next? Accessing the right training for safe medication
Training is important in the safe administration of medication.
Well-trained workers know how important it is to give the right medication. They will write down everything correctly and help each other take time to give the medication safely.
Our Safe Administration of Medicines course can be taught as an open course, or brought to your care setting.
In addition if your clients use peg feeding, we would recommend them partaking in that course. We will discuss and practice the specifics around enteral tube feeding.
Taught by registered nurses, staff will learn about their
- responsibilities,
- about medication errors,
- infection control and risk assessment,
- how to administer medication, and
- ensure correct documentation and disposal of medication.
For more information, or to arrange a course for your staff, contact us on 01782 563333 or email office@caringforcare.co.uk.
LATEST POSTS
- Understanding Bereavement Support and Duties of Different Healthcare Groups.
- What are Vital Signs in Nursing?
- Hoist Training for Carers: Ensuring Safe and Efficient Patient Transfers
- Power of Person-Centred Care: Putting Patients First for Better Outcomes
- Understanding Drug and Alcohol Testing in the Workplace
Let us Help you
We’ll help you find the right course for your needs. Tell us a little bit about your situation and what you would like to achieve.
We’ll get back to you within one working day.
