Statutory And Mandatory Training: Important Things To Know
As healthcare professionals, we get bombarded with seemingly endless compliance training requirements on top of our patient care duties.
From information governance to health and safety, the sheer volume of required modules can feel daunting.
This guide will clearly define “statutory” versus “mandatory” requirements, explain common topics, provide learning tips, and most importantly, discuss how these two training requirements ultimately aim to protect us and our patients.
Together we’ll make sense of these learning obligations in service of providing safer, higher quality care.
Table of contents
- Defining Statutory and Mandatory Training
- Why Healthcare Organisations Mandate Training
- What is the mandatory and statutory practical training course?
- Common Statutory and Mandatory Training Topics
- Learning Requirements by Staff Role
- Organisation Training: Equipping Learners for Success
- Supporting Training Transfer Back to the Workplace
- Avoiding Training Fatigue from Overload
- Closing the topic
- Statutory and Mandatory Training FAQs
Defining Statutory and Mandatory Training
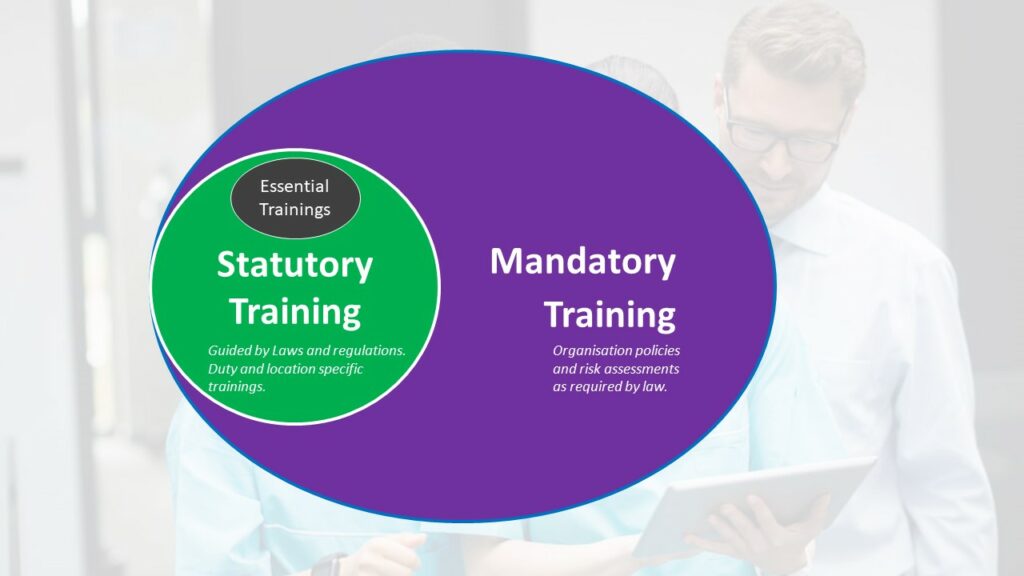
What’s the difference between statutory and mandatory training?
Statutory training refers to training that is required by specific laws and regulations. Mandatory training encompasses training required by organisational policies, risk assessments, and procedures. All statutory training would be considered mandatory, since organisations must comply with relevant laws.
But some additional training may be mandatory for a given role or workplace without being legally required for all healthcare providers.
Let’s first decode these two terms which are often used interchangeably:
Statutory Training:
- Required by specific laws and regulations like the Health and Safety at Work Act.
- Developed and regulated by government agencies.
- Often has defined minimum course content and durations.
- Usually requires accredited training.
Mandatory Training:
- Required by the employer rather than direct legislation.
- Based on organisational policies and risk assessments.
- May cover a broader range of topics like soft skills.
- Defines local standards and best practices.
- Can use non-accredited proprietary content.
All statutory training is mandatory, but not all mandatory training is statutory.
Think Venn diagram with overlap. We’ll explore common examples shortly.
Why Healthcare Organisations Mandate Training
Leaders often get questions on why certain modules are deemed mandatory. Reasons include:
- Meeting regulatory requirements from bodies like the Care Quality Commission and NHS England.
- Standardising staff capabilities and care quality across locations.
- Reducing organisational risks like penalties, lawsuits and revoked contracts.
- Protecting staff and patient health, safety and wellbeing.
- Addressing high vulnerability areas identified by risk assessments.
- Ensuring use of technologies like health IT systems and equipment.
- Onboarding new joiners on organisational policies and protocols.
- Maintaining insurance coverage that requires training documentation.
- Reinforcing a culture of continual improvement and care excellence.
While mandating some learning seems burdensome, reasons like reducing harm make requirements worthwhile.
What is the mandatory and statutory practical training course?
This refers to hands-on, practical courses focused on training needs with a statutory or legal mandate, as opposed to just theory or awareness.
Examples include practical sessions for manual handling, basic life support, infection control procedures, and fire safety response.
Employers must ensure healthcare professionals receive practical instruction and assessment on these critical risk areas per healthcare regulations.
Common Statutory and Mandatory Training Topics
While varying somewhat by specialty, typical required training modules cover:
- Basic Life Support / CPR
- Health and Safety
- Fire Safety
- Infection Control
- Information Governance
- Safeguarding Adults
- Safeguarding Children
- Mental Capacity Act and Consent
- Dementia Awareness
- Mental Health Act
- Conflict Resolution
- Diversity and Inclusion
- Customer Service
- Food and Nutrition
Let’s explore some prominent examples in more detail.
Basic Life Support Training
Basic life support skills enable rapid response to breathing and cardiac arrests in that critical first few minutes before experts can come to help.
Required training ensures we can provide potentially lifesaving assistance when emergencies strike.
Common BLS training topics include:
- Assessing consciousness
- Recovery position
- Performing chest compressions
- Clearing airways and rescue breathing
- Using AED defibrillators
- Managing choking
- Calling for emergency assistance
Some healthcare professionals like doctors and nurses require more advanced life support training for interventions like medications and advanced airways.
But core skills like high-quality CPR make BLS training mandatory for all direct care providers.

A 2020 study by the NHS Improvement found that statutory training on fire safety can improve evacuation procedures and reduce the risk of fire-related incidents in healthcare settings.
Fire Safety Training
Catastrophic facility fires remain one of the highest hazard risks in healthcare.
Mandatory fire training prepares us to contain fires, safely evacuate, and prevent their ignition in the first place.
Standard fire training instruction covers:
- Facility fire safety features – alarms, exits, extinguishers, sprinklers.
- Fire chemistry and using different extinguisher types.
- PASS – proper extinguisher use technique.
- Roles when fire alarms activate – containment, evacuation support, roll calls.
- Hazards increasing fire risk that must be reported.
- Fundamentals of prevention – storage, oxygen, smoking policies.
Fire drills applying learning in situ are key to responding instinctively when real emergencies strike.
Infection Control Training
Preventing the spread of infections protects both healthcare workers and vulnerable patients. Typical infection control modules include:
- Hand hygiene – washing, sanitiser use.
- Isolation – PPE donning and doffing, types of precautions.
- Disinfecting equipment and environment.
- Sharp safety – engineered devices, disposal.
- Waste streams – sorting different hazard levels.
- Exposure management – needlestick protocols, prophylaxis.
- Immunisation – healthcare worker requirements.
- Reporting responsibilities – exposure incidents, outbreaks.
Reinforced hygiene habits like thorough hand washing between patients prevents countless transmissions.
Mental Capacity and Consent
Obtaining proper consent honors patient rights and promotes ethical care.
Key content areas are:
- Legal definition of capacity – ability to understand, retain and weigh information to make decisions.
- Assessing capacity and documenting rationally.
- Identifying impairments affecting capacity – dementia, delirium, intoxication, developmental disability.
- Vulnerable groups requiring protection.
- Steps if patients lack capacity – involving advocates, best interest decisions.
- Types of medical consent.
- Requirements for informed consent – disclosure, comprehension, voluntary choice.
- Consent documentation.
Getting really good at talking about consent stops misunderstandings that can go against what patients want and create problems.

A 2018 study by the Royal College of Nursing (RCN) found that mandatory training on medication administration can reduce medication errors by up to 30%.
Some examples of training required by statute in healthcare settings include:
1. Fire safety training mandated under Regulatory Reform (Fire Safety) Order 2005.
2. Health and safety training required by Health and Safety at Work Act 1974.
3. Data protection and information governance training complying with Data Protection Act 2018.
4. Safeguarding training dictated by various child and vulnerable adult protection laws.
5. First aid training fulfilling the Health and Safety (First Aid) Regulations 1981.
Learning Requirements by Staff Role
While many modules are universal, certain designated training is mandated based upon roles:
- Nurses: I.V. therapy, blood administration, catheterisation, tracheostomy care, restraints
- Doctors: Conscious sedation, central lines, lumbar punctures.
- Pharmacists: Medication reconciliation, high-risk drug safeguards, immunisation
- Radiology Staff: Radiation protection, MRI safety, contrast risks.
- Facilities Staff: Hazardous chemicals handling, instrument sterilisation, medical gas storage
- Food Services: Food allergies, texture modifications, infection control.
Customised learning to environment and duties makes sure healthcare workers have the skills they need for their usual tasks and the challenges they might face.
BECOME CERTIFIED – ONLINE MANDATORY CARE TRAINING COURSES – CLICK HERE
Organisation Training: Equipping Learners for Success
How should organisations prepare staff for mandatory learning?
Ideas include:
- Providing training schedules well in advance for planning.
- Reserving protected time for training away from direct duties.
- Offering training at flexible times – nights, weekends, online.
- Developing training aids like handbooks, videos and job aids.
- Building in discussion periods to exchange real-world applications.
- Ensuring staff understand the “why” behind requirements.
- Offering overtime incentives and food for extra training shifts.
- Providing central training spaces conducive to learning.
- Arranging backfill and cross-training to cover workload during training.
Understanding expectations and receiving support to fulfill them enables learners to embrace requirements.
We recommend that a member of your team attends a specific train-the-trainer course to gain a better understanding of how to handle training for your organisation. This would provide a clear approach to developing and delivering effective training programs.
Presentation Approaches That Engage Learners
Well-crafted education experiences make mandated modules more motivating and sticky.
Consider:
- Starting with powerful stories underscoring why the issue matters. Appeal to emotions.
- Using humor judiciously while retaining professional focus. Avoid sarcasm.
- Incorporating quick polls, quizzes and team games to maintain energy.
- Building in videos, roleplays and hands-on simulations for interactivity.
- Sharing real examples from news and organisational experience to increase salience.
- Discussing likely pain points upfront that modules aim to prevent.
- Allowing brief peer discussion of times training would have helped.
- Asking teams to draft potential practice improvements from concepts.
- Reviewing key points frequently for memorability.
- Ending with an inspirational summary motivating behaviour change.
Thoughtful engagement strategies make mandated training feel more purposeful than passive.
Participation Tracking and Follow-Up
Consistent compliance monitoring ensures training translates into practice:
- Maintain training records with assignment dates and completion status.
- Track skills assessments where applicable – CPR testing, moving and handling skills, demonstrations.
- Notify when renewals are nearing due dates and schedule training.
- Run routine compliance reports for leadership review.
- Develop correction plans for repeated unmet requirements like coaching or progressive discipline.
- Survey workers on effectiveness translating training to actual practice.
- Observe performance periodically assessing training incorporation.
- Provide reminders like posters and quick reference guides reinforcing key messages and techniques.
What gets monitored gets managed. Gentle compliance nudges work better than penalties.
Supporting Training Transfer Back to the Workplace
Classrooms must connect to clinical care to achieve outcomes:
- Provide printed takeaway job aids and resources on taught concepts. Prevent forgetting.
- Develop peer support networks for learners to exchange successes and hurdles applying new techniques or protocols.
- Ask participants to draft potential practice improvements from concepts learned.
- Have managers discuss new learnings and how they can be applied in the work unit.
- Recognise individuals demonstrating successful training application.
- Conduct manager rounding to get staff input on training utilisation barriers and needs.
- Host periodic refresher talks and lunch-and learns reinforcing core lessons.
Without support for integration into hectic workflows, concepts taught can too easily be forgotten.
BOOK PRACTICAL COURSES – SEE ALL FACE TO FACE PRACTICAL COURSES – CLICK NOW
Avoiding Training Fatigue from Overload
Training overload demotivates rather than activates learning.
Principles to prevent training overload include:
- Group related lessons together, learning them slowly and in a way that makes sense, instead of throwing a bunch of random courses all at once.
- Refresh only essential portions annually after initial comprehensive onboarding modules. Avoid full repeats unnecessarily.
- Blend learning formats – online modules for knowledge plus in-person skill practice rather than hours of straight lecture.
- Use microlearning formats like podcasts and infographics to convey bite-sized concepts.
- Vary delivery – videos, serious gaming, peer teach-backs.
- Discuss early with managers to spread required modules across the annual schedule rather than cramming at year-end.
- Offer training credit for related external learning like conference sessions.
- Create central FAQs on training requirements to cut through confusion.
While extensive, requirements can feel manageable when thoughtfully coordinated, formatted and delivered.
Closing the topic
We hope this guide helps provide reassuring rationale for the safety and compliance training we undertake as healthcare professionals.
While burdensome at times on top of our duties, the shared goal of protecting patients ultimately makes requirements worthwhile.
We shoulder these obligations together for the greater good.
By embracing mandated training with grace and purpose, we elevate care quality, colleague support, and public trust in our noble profession.
Our learning truly lifts all when we recognise its deeper connections to safety and excellence.
For advice on training needs, please talk to our team 01782 563333 or send us an email: enquiries@caringforcare.co.uk.

A 2017 study by the National Health Service (NHS) England found that mandatory training on infection prevention and control (IPC) can reduce healthcare-associated infections (HAIs) by up to 50%.
Statutory and Mandatory Training FAQs
Statutory requirements form a subset of overall mandatory training, so the terms are not fully interchangeable.
Think of mandatory as the larger umbrella encompassing all compulsory employer-required training.
The component that is legally required by specific regulations makes up statutory training.
So all statutory training is mandatory, but not all mandatory training is statutory.
Care homes have a range of core statutory and mandatory training requirements for their staff under CQC guidelines and health and safety laws.
Common subjects include safeguarding, mental capacity, infection control, moving and handling, food safety, fire safety, first aid, health and safety, medication management, and data protection.
Refresher frequencies are often set annually or every 3 years.
Common statutory trainings cover fire safety, health and safety, first aid, safeguarding, Mental Health Act, Mental Capacity Act, deprivation of liberty, food safety, hazardous materials, and infection control.
The specific subjects and frequencies are dictated by laws like Health and Safety at Work Act, Food Safety Act, and data protection regulations.
Let us Help you
We’ll help you find the right course for your needs. Tell us a little bit about your situation and what you would like to achieve.
We’ll get back to you within one working day.
